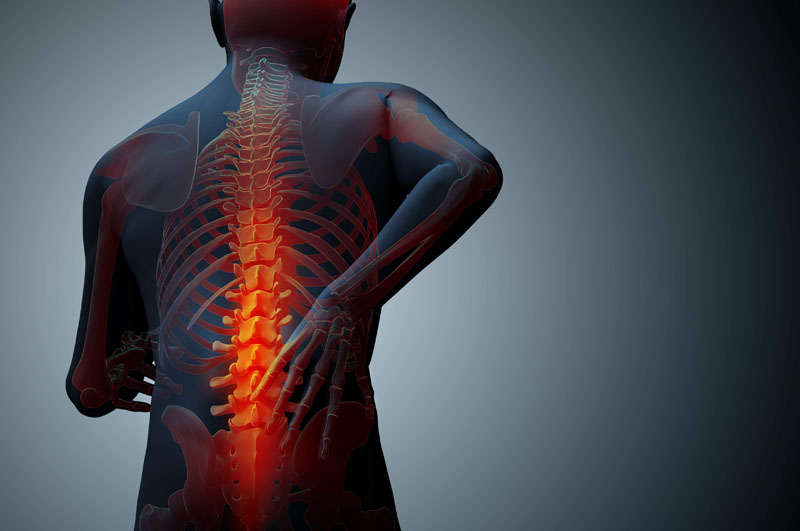
Back pain is a prevalent issue that affects millions of people worldwide, impacting their quality of life and overall well-being. As one of the leading causes of disability and missed workdays, it is essential to gain a comprehensive understanding of the common factors that contribute to back pain. In this article, we will delve into the valuable insights provided by Dr. Ganesh Mundhe, a renowned back pain specialist, to shed light on the various causes of back pain and how his expertise can help patients find effective solutions.
Poor Posture and Sedentary Lifestyle:
Dr. Ganesh Mundhe emphasizes that poor posture and a sedentary lifestyle are significant contributors to back pain. Prolonged hours of sitting, whether at a desk or in front of a screen, can lead to weakened back muscles and strained ligaments, resulting in discomfort and pain. Understanding the importance of maintaining proper posture and incorporating regular physical activity into daily routines can help prevent and alleviate back pain.
Muscle Strain and Injury:
Muscle strains and injuries are common culprits behind acute back pain. Lifting heavy objects incorrectly, sudden movements, or engaging in strenuous physical activities without proper warm-up can lead to muscle tears or sprains in the back. Dr. Ganesh Mundhe advises patients to practice proper lifting techniques, avoid overexertion, and participate in regular exercise programs that strengthen the back and core muscles.
Degenerative Disc Disease:
Degenerative disc disease is a condition that occurs with age and involves the natural wear and tear of the spinal discs. As the discs lose their cushioning properties, they can cause compression of the nerves and lead to chronic back pain. Dr. Ganesh Mundhe stresses the importance of maintaining a healthy lifestyle, including a balanced diet and regular exercise, to minimize the impact of degenerative disc disease on the spine.
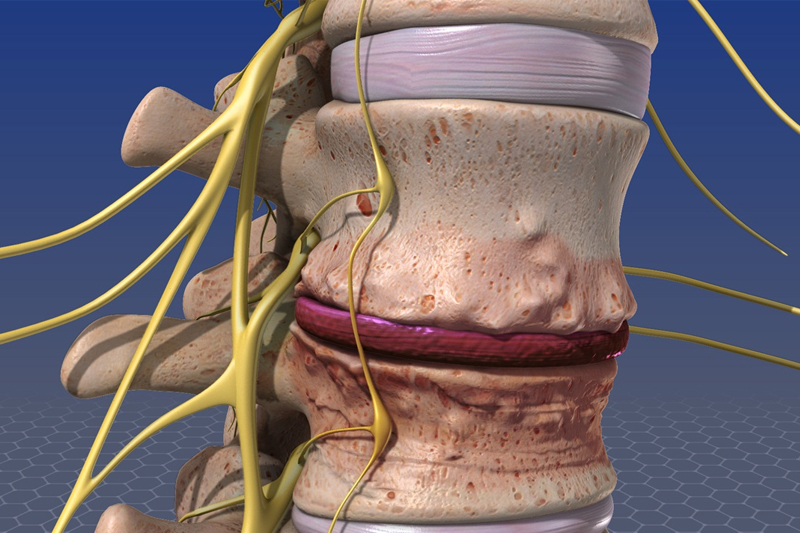
Herniated or Bulging Discs:
A herniated or bulging disc occurs when the soft cushion-like material between the spinal vertebrae pushes out and presses against nearby nerves. This can result in shooting pain, tingling, or numbness down the legs, a condition known as sciatica. Dr. Ganesh Mundhe offers specialized treatments such as spinal adjustments and therapeutic exercises to relieve pressure on the affected nerves and provide relief.
Arthritis and Spinal Stenosis:
Arthritis, particularly osteoarthritis, can affect the joints of the spine and lead to chronic back pain. Additionally, spinal stenosis, a narrowing of the spinal canal, can cause pressure on the spinal cord and nerves, resulting in discomfort and reduced mobility. Dr. Ganesh Mundhe utilizes a multidisciplinary approach to manage arthritis-related back pain, combining chiropractic care, physical therapy, and lifestyle modifications.
Stress and Emotional Factors:
Stress and emotional factors can have a surprising impact on back pain. Tension and anxiety can lead to muscle tension and pain in the back and neck. Dr. Ganesh Mundhe emphasizes the importance of stress management techniques, such as meditation, yoga, or counseling, to help alleviate back pain caused by emotional factors.
Understanding the common causes of back pain is crucial in finding effective solutions to alleviate discomfort and improve overall spinal health. As highlighted by Dr. Ganesh Mundhe, addressing poor posture, incorporating regular physical activity, and seeking professional guidance for specialized treatments are essential steps to managing back pain. By taking a proactive approach to back health, individuals can enhance their quality of life and enjoy a pain-free and active lifestyle. If you are experiencing back pain, do not hesitate to consult Dr. Ganesh Mundhe, who offers compassionate care and tailored solutions to help you find relief and regain your well-being.
Get effective back pain treatment in Pimple Saudagar from Dr. Ganesh Mundhe. Our expert chiropractic care specializes in lower back pain treatment, providing tailored solutions for lasting relief and improved spinal health. Regain your mobility and well-being with personalized care from Dr. Ganesh Mundhe, your trusted back pain specialist in Pimple Saudagar.